This article was published in 2016. To maintain an accurate record of our history, we have kept references to previous organisation names and terms such as New Zealand AIDS Foundation, Ending HIV and Love Your Condom.
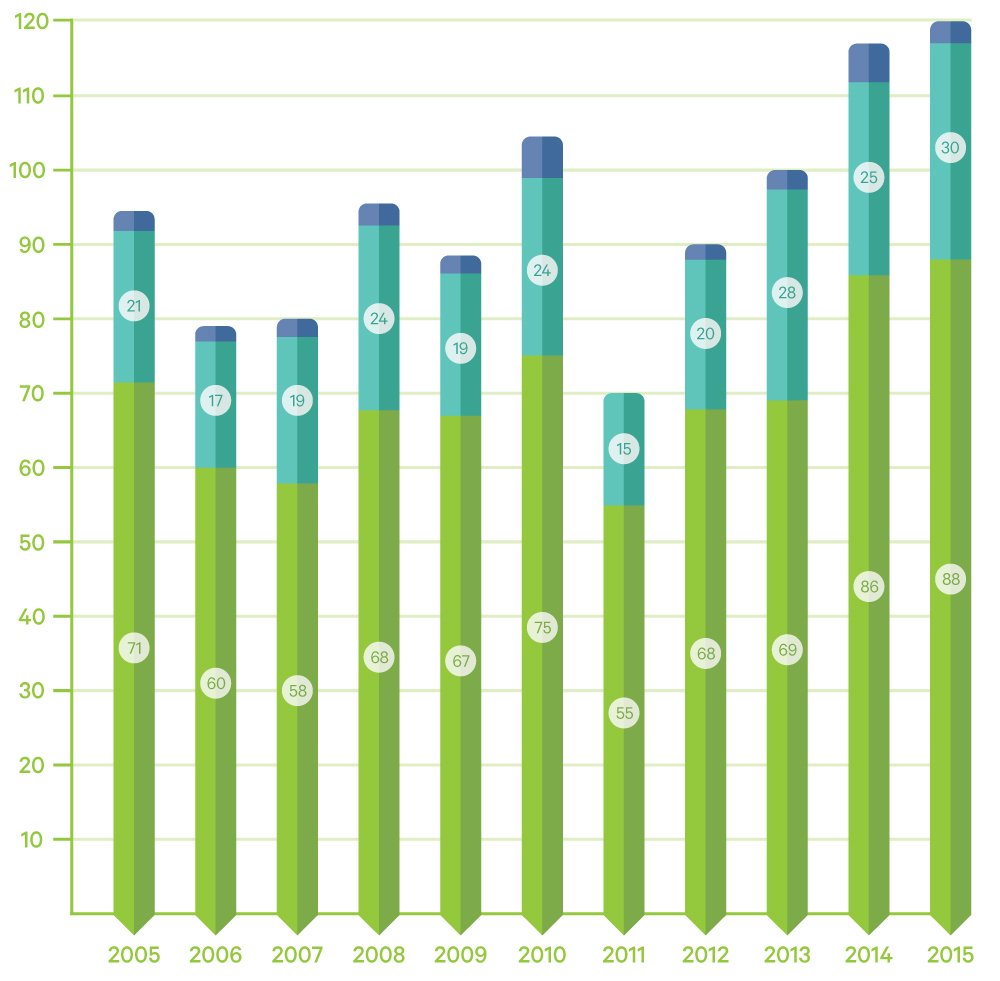
Latest figures show that 2015 had the highest number of newly diagnosed HIV infections among gay and bisexual men ever recorded.
- 88 gay and bisexual men were diagnosed as having contracted HIV in New Zealand compared to 86 in 2014.
- A further 32 gay and bisexual men were infected overseas or the place of infection was unknown; a total of 120 who were first diagnosed in New Zealand.
- Another 36 heterosexual men and women were first diagnosed with HIV in New Zealand in 2015, two less than in 2014.
- A total of 185 people were first diagnosed with HIV in New Zealand, and an additional 39 had previously been diagnosed overseas.
- 58% of gay and bisexual men diagnosed in 2015 had a low CD4 cell count which indicates they had been living with the virus long term. This is an increase from 53% in the previous year.
Annual HIV diagnoses in gay and bisexual men in New Zealand 2005-2015 (excludes those previously diagnosed overseas)
Latest figures by University of Otago’s AIDS Epidemiology Group show the number of gay and bisexual men living with long-term undiagnosed HIV may be reducing, but, the epidemic is making a comeback with increasing new infections. More needs to be done.
“The trend is concerning and shows the urgent need for a re-energised response to HIV in New Zealand, including Government’s commitment to make available the new tools that can stop HIV in its tracks,” said Nick Laing, acting Executive Director of the New Zealand AIDS Foundation (NZAF).
“New Zealand’s HIV epidemic is relatively small by international standards but that is not good enough,” said Mr. Laing. “High condom use has kept the HIV prevalence low but it is clear that condom promotion alone will not stop HIV. We need significantly more testing throughout the health system, the removal of PHARMAC’s CD4 threshold so that people can access treatment as soon as they are diagnosed and funding for PrEP, a daily pill that can prevent HIV infection.”
Testing has become more important than ever in the response to HIV. Based on data from Otago University’s AIDS Epidemiology Group it is estimated that approximately 640 people live with HIV in New Zealand and don’t yet know it, the majority of whom are gay and bisexual men.
“We can expect that the annual number of diagnoses among this group will continue to rise over the next several years as efforts to increase rates of testing and reduce the number of undiagnosed are scaled up.”
In 2015, NZAF services conducted a total of 3819 free rapid HIV tests. This was a 42% increase on the number of tests conducted in 2014 and a 75% increase on two years ago.
Reducing the number of people living with undiagnosed HIV infection and enabling them to start treatment as soon as possible has a significant impact on driving down rates of new infection. Most people who are on treatment reach an undetectable viral load which drastically reduces the risk of passing on the virus.
“We are doing all we can to promote condoms and increasing our testing as much as possible but the government must step up if infections are to be stopped. The New Zealand AIDS Foundation cannot provide all the testing that is needed. GPs, hospitals and sexual health services can make HIV testing a higher priority. Once someone is diagnosed with HIV they should be able to access treatment immediately.”
Recently, the Government announced $124 million to be made available for PHARMAC and NZAF strongly believes that some of the funding needs to go towards removing the outdated CD4 threshold. This currently denies hundreds of Kiwis who have been diagnosed with HIV from accessing medication until their immune system is significantly damaged.
An example similar to New Zealand would be Denmark where the CD4 threshold was removed in 2006 and their testing programme was scaled up. As a result, new infections are now dropping steadily in Denmark. This can be achieved in New Zealand too.
Otago University’s AIDS Epidemiology Group has recommended that pre-exposure prophylaxis (PrEP), a daily pill that can prevent HIV infection, should be considered for those at highest risk of HIV.
“We agree with this recommendation that PrEP is a highly-effective prevention option for some people and it needs to be funded,” said Mr. Laing. “There is consensus around the world that these are the combination of actions that can end HIV. It is what the World Health Organisation has recommended. The fact that we have seen another year of increased new infections means that government needs to act urgently to bring New Zealand’s response to HIV up to speed,” said Mr. Laing.

