This article was published in 2019. To maintain an accurate record of our history, we have kept references to previous organisation names and terms such as New Zealand AIDS Foundation, Ending HIV and Love Your Condom.
The New Zealand AIDS Foundation calls for more healthcare providers to understand the role of PrEP in NZ’s HIV response and encourages more practitioners to understand the process to prescribe it.
New Zealand needs more clinicians prescribing PrEP (Pre-Exposure Prophylaxis) to maximise its public health efficacy and to ensure there are plenty of health touchpoints to accessing PrEP for those most at risk of contracting HIV. This will, in turn, contribute to increased equitable access for people at-risk.
PrEP is the use of specific antiretroviral treatments (emtricitabine and tenofovir) by HIV-negative people to prevent HIV acquisition. When taken as prescribed, PrEP can reduce the risk of contracting HIV by up to 99%, even when condoms aren’t being used.
A lot of clinicians may have heard more about PrEP since it became funded by PHARMAC in 2018, but there is a need to progress from awareness through to being able to prescribe.

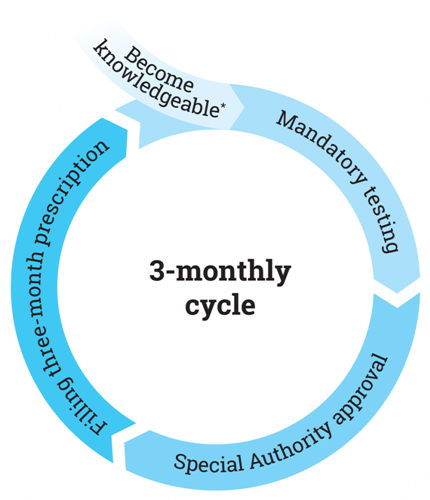
A mapped journey for healthcare providers and PrEP could look like this
A mapped journey for healthcare providers and PrEP could look like this
NZAF asked what might be stopping GPs from progressing through this journey to become prescribers of PrEP.
The leading reported barriers were:
- The process appearing too complicated
- Unknown, or increased, impact on the capacity of the practice
Addressing these barriers and overcoming them is the next step in effectively responding to the HIV epidemic here in New Zealand. By increasing access to PrEP, the healthcare system is taking an important step toward ending new HIV transmissions.
NZAF Chief Executive Dr Jason Myers says equitable PrEP access and uptake is one of the key pillars of the HIV response in New Zealand.
“PrEP has the potential to really change the game here in New Zealand. We’ve already seen good uptake of the prevention strategy but we need to scale this up if PrEP is to reach full potential. We often hear that patients can give up on pursuing PrEP because their local practice was not prescribing it, so we are wanting to increase the number of practitioners who are interested in and knowledgeable about PrEP around New Zealand,” says Dr Myers.

New Zealand AIDS Foundation Chief Executive Dr Jason Myers
New Zealand AIDS Foundation Chief Executive Dr Jason Myers
How to prescribe PrEP in New Zealand
*If anyone would like to start their journey to prescribing PrEP – they can head here to become a key part of New Zealand’s HIV response.
1. To begin with, all it takes is a desire to learn about PrEP
This can be done by:
-
- Completing the online learning module: Practical PrEP Guidance for GPs in New Zealand (40 minutes)
- Completing an accredited PrEP-prescribing course like those offered by bpac.org.nz
- Reading through ASHM’s PrEP guidelines
- Personal research
All of these resources and more can be found here.
If a clinic would like to be listed on the PrEP Prescribing Doctors map, there is a form at the bottom of this page.
2. Pre-treatment testing – confirm HIV negative status and run full STI screen (rectal & throat swabs, urine test, HIV, syphilis and hepatitis), as well as kidney and liver function tests at baseline – no more than 2 weeks prior to approval application
3. Special Authority approvals – these are written on a per-patient basis and are renewed three-monthly, this includes:
-
- A named HIV specialist endorsement of referral
- Confirming patient meets PHARMAC criteria checks
- Once the application is approved, prescriptions can be issued and the next appointment should be booked in to take place in 3-months. This is to perform mandatory tests and check in with the patient

A list of contact details for clinics with access to named HIV specialists
A list of contact details for clinics with access to named HIV specialists
It can be that simple.
Simple doesn’t mean slack
Though this process is simplified – it has been made so to encourage rapid uptake – it doesn’t mean this is a rushed or relaxed system.
PrEP is a commitment to a health regimen from both patient and prescriber.
Funded PrEP requires three-monthly check-ups to write repeat prescriptions, carry out a full range of screenings and check in with the patient about wellbeing, adherence or any concerns.
The increase in appointments needed to ensure an effective service will require that a clinic’s infrastructure is able to accommodate the extra visits and tests. This is an important part of moving New Zealand closer to ending new HIV transmissions. A little admin, for a lot of beneficial outcome.
Increasing the number of PrEP prescription services will mean more supportive healthcare options for those at most risk of HIV, as well as wider public health benefits for the country.
- Increased screenings mean more touchpoints to identify and treat other STIs – potentially improving control of gonorrhoea, chlamydia and syphilis as well as HIV
- More clinics providing this service around the country could mean more opportunities for equitable access for Māori, Pacific and Asian MSM
- Increased discussions around sexual health and risk could mean a more educated sexually active population and opportunities for intervention
- More effective PrEP services for at-risk MSM could also improve the way primary healthcare meets the needs of non-heterosexual and transgender patients generally
“Short of a vaccine against HIV, PrEP could be the best opportunity for primary care to eliminate HIV transmission in New Zealand. Imagine that – no more new infections! A few simple steps can get us there: know who your MSM patients are; offer prevention options, and follow up regularly. Every conversation you have moves NZ closer to ending HIV,” says, Director of Gay Men’s Sexual Health Research Group, University of Auckland, Dr Peter Saxton.

Director of Gay Men’s Sexual Health Research Group, University of Auckland, Dr Peter Saxton
Director of Gay Men’s Sexual Health Research Group, University of Auckland, Dr Peter Saxton
Being PrEPared - minimising impact on the practice
The unknown impact of prescribing PrEP out of a practice is a commonly reported barrier to beginning to prescribe the HIV prevention medication.
NZAF spoke to Dr Torrance Merkle of Hobsonville Family Doctors about how PrEP prescription has been effectively implemented in their practice.
“I’ve found that my PrEP patients are actually willing to do a lot of the initial work themselves. They tend to be relatively informed about PrEP and get the hang of making sure they are booked in for review 1-2 weeks before they run out. For first consults, I use a typing template, so I know we’ve discussed and documented everything.
“We did some brief education with our nurses so they knew there would be a slight increase in testing needs and why – this way they’re informed and know the deal. It just becomes a part of the routine. Our nurses are also more confident doing sexual health checks for MSM, if needed in between their PrEP visits.
“Our clinic has found the most efficient way of doing PrEP repeats is for the patient to book in 1-2 weeks before their script is due, so they don’t run out. In the consult the Doctor can do the throat swab and supply the urine test and rectal swabs for the patient to do next. We then offer for the nurse to do their blood test (for a fee) to save them having to travel and wait at the lab. I usually text results through within a day or two, along with confirmation that I’ve renewed the special authority.
“I’d say that prescribing PrEP is actually simpler than many other presentations we see as GPs – although there are a few risks and things to monitor, there are huge benefits to individual patients and the community in terms of preventing HIV transmission. If prescribing several patients this medication prevents even a single case of HIV acquisition, then we’re doing our job.
“A comparison could be drawn with the combined contraceptive pill – it just requires a discussion of risks and benefits to the patient, and making sure they understand enough to make an informed decision. Although there tends to only be one consultation per year for the pill, there are usually only four check-ins with PrEP patients which can definitely be managed.”
“I’ve found that offering PrEP has been really rewarding, as you get to know patients really well when you meet them every three months!”
Four ways to prepare to begin prescribing PrEP:
- Speak to a named HIV specialist before submitting the first Special Authority application (or in Auckland, send an eReferral to Sexual Health with all the details and baseline lab results). Check what their process and expected turnaround timelines are and make any general enquiries then and there - to ensure the practice is well equipped for when that first patient walks through the door.
- Talk to staff about PrEP, especially relevant teams who will become a part of the process. Brief nurses on the tests needed for a patient seeking PrEP, let admin staff know about the three-monthly appointment requirements. If it is a shared practice, speak with the other practitioners about the intention to prescribe PrEP and gauge whether they are also willing to learn about prescribing PrEP – at the very least to notify them that there may be a slight increase in patients registering.
- Logistics. Prescribing PrEP means setting up recurring three-monthly appointments, prompting patients to source or organising required tests within 1-2 weeks of renewing or initially prescribing and being available for those appointments. Beyond that, it’s only a little extra paperwork.
- Keep in mind the population who are most at risk of HIV and eligible for PHARMAC funded access to PrEP (men who have sex with men and transgender people) is reasonably small – with an increase in the number of practices that offer PrEP, it’s likely the caseloads from within this population will be shared even further. This means it is unlikely that an unmanageable number of patients will be approaching each practice for help getting on PrEP.
If this sounds like something your practice could start implementing – head to nzaf.nz/prescribePrEP to find more support resources and tools to help get started.
The PrEP-Prescribing Doctors Map
The PrEP-Prescribing Doctors Map is a great way to be visible to patients and show that a practice caters to the needs of MSM.
NZAF Health Services Regional Manager Alex Anderson says connecting people to PrEP is a large part of the requests that come through its clinics.
“Having worked in both clinical spaces and with NZAF, I see the importance of ensuring equitable access to PrEP prescriptions is simple for both prescriber and patient. What we know of MSM is that not all of them are “out” or open with their healthcare providers, so it can be hard to even begin conversations around PrEP. Having a practice listed on the ‘PrEP Map’ means patients can see a range of local practices that are more likely to be able to meet their needs and will hopefully result in fewer instances of discrimination or negative experiences when describing sexual behaviours to doctors,” he says.

PrEP-prescribing doctors map - overview
PrEP-prescribing doctors map - overview
Those already prescribing PrEP and listed on this resource are encouraged to let peers know how simple this process can be and help others to effectively implement PrEP prescription in their practices.
Find out more and be a part of connecting those most at risk of HIV to a valuable prevention tool - click here.

